Gut Check: How I Learned to Listen to My Stomach (And You Should Too)
Ever felt bloated after a meal that should have been fine? Or had stomach issues pop up out of nowhere? I’ve been there—constantly. What changed wasn’t a miracle cure, but learning how to assess my gut health in real, practical ways. Turns out, your stomach talks if you’re willing to listen. This is how I started paying attention, testing small changes, and actually seeing results worth sharing. Gut health isn’t just about avoiding discomfort—it’s about tuning in to one of your body’s most honest communication systems. And for many women in their 30s, 40s, and 50s, who juggle family, work, and personal well-being, understanding this connection can be life-changing.
The Silent Alarm: Recognizing When Your Gut Is Off
Many people dismiss stomach discomfort as an unavoidable part of daily life. A little bloating after dinner? Normal. Occasional heartburn? Just spicy food. Fatigue after lunch? Must be the weather. But these symptoms are not random inconveniences—they are signals. The digestive system is highly sensitive, and when it’s out of balance, it sends messages long before serious conditions develop. Common signs like persistent bloating, gas, irregular bowel movements, or feeling unusually tired after eating are not quirks—they are clues.
For example, bloating that occurs consistently after meals may point to food intolerances, poor digestion, or imbalances in gut bacteria. Acid reflux that happens more than once a week could indicate gastroesophageal reflux disease (GERD), especially if it worsens when lying down. Stool consistency—whether too hard, too loose, or inconsistent in shape—can reflect hydration levels, fiber intake, or even stress. The Bristol Stool Chart, a medically recognized tool, helps categorize bowel movements from type 1 (separate hard lumps) to type 7 (watery, no solid pieces). Types 3 and 4 are considered ideal, indicating healthy digestion and proper transit time.
What makes these symptoms so easy to ignore is their gradual onset. They rarely appear suddenly with dramatic intensity. Instead, they creep in—slightly more bloating, slightly longer digestion, slightly more fatigue—and over time, the body adapts. This adaptation creates a false sense of normalcy. But the gut does not lie. When digestion is compromised, nutrient absorption suffers, inflammation can increase, and energy levels drop. Recognizing these early warnings is the first step toward meaningful change. It’s not about chasing perfection but about restoring balance.
Why Gut Health Isn’t Just About What You Eat
Diet is undeniably important, but it’s only one piece of the digestive puzzle. Many women focus solely on food choices—cutting sugar, increasing fiber, avoiding processed items—yet still struggle with stomach issues. The reason? Other lifestyle factors play a powerful role in how the gut functions. Stress, sleep quality, hydration, and even meal timing influence digestion as much as, if not more than, the food itself.
Take stress, for instance. When the body is under emotional or mental strain, it activates the sympathetic nervous system—the “fight or flight” response. This physiological state slows down digestion. Cortisol, the primary stress hormone, reduces blood flow to the digestive tract and suppresses stomach acid production. As a result, food sits longer in the stomach, leading to bloating, gas, and discomfort. This is why many people notice stomach issues flare up during busy seasons at work, family conflicts, or periods of emotional upheaval—even if their diet hasn’t changed.
Sleep is another critical factor. The gut has its own circadian rhythm, synchronized with the body’s internal clock. Poor or irregular sleep disrupts this rhythm, affecting the balance of gut bacteria. Studies show that people who consistently sleep less than six hours per night have lower microbial diversity—a key marker of gut health. Hydration also plays a direct role. Water is essential for breaking down food, absorbing nutrients, and moving waste through the intestines. Even mild dehydration can slow digestion and contribute to constipation.
Meal timing matters too. Eating too quickly, skipping meals, or consuming large portions late at night forces the digestive system to work inefficiently. The body is designed to digest food best during daylight hours, when metabolic activity is highest. Late-night eating can lead to indigestion and poor nutrient absorption. Understanding these non-dietary influences shifts the focus from blame to awareness. It’s not always about eating the “perfect” meal—it’s about creating the right conditions for digestion to thrive.
Simple Self-Checks You Can Do at Home
You don’t need expensive tests or a medical degree to start understanding your gut health. Simple, everyday observations can reveal a lot about how your digestive system is functioning. The key is consistency and attention to detail. One of the most effective tools is a symptom journal. This doesn’t have to be complicated—a notebook or notes app works perfectly. Each day, record what you eat, when you eat, and how you feel afterward. Note any bloating, gas, energy levels, or bowel movements.
Over time, patterns begin to emerge. For example, if you notice bloating two hours after eating dairy, that could indicate lactose intolerance. If fatigue follows meals high in refined carbohydrates, it might suggest blood sugar fluctuations affecting digestion. Delayed symptoms—those that appear hours after eating—are often overlooked but can be highly revealing. Immediate reactions, like heartburn right after a meal, are easier to connect to food, but delayed responses require tracking to identify.
Another useful self-check is observing bowel movement frequency and form. Tracking this for a week can provide insight into digestive transit time and overall gut function. Regularity varies from person to person, but going less than three times a week may indicate constipation, while more than three loose stools daily could suggest irritation or imbalance. Noting color is also helpful—pale stools may point to bile issues, while dark stools could signal upper digestive bleeding and should be evaluated by a doctor.
Energy levels after meals are another valuable clue. Ideally, you should feel energized, not sluggish, after eating. If you consistently feel tired or foggy after meals, it could mean your body is struggling to digest or absorb nutrients efficiently. This is especially common with large, heavy meals or those high in fat and sugar. By paying attention to these subtle signals, you gain a clearer picture of your digestive health without stepping into a clinic. These observations also become powerful tools when speaking with a healthcare provider, offering concrete data instead of vague descriptions.
The Food-Mood Connection: Tracking Triggers Without Guesswork
Not all foods affect everyone the same way. What’s healthy for one person might cause discomfort for another. This is especially true for common irritants like dairy, gluten, caffeine, and spicy foods. Many women assume these items are fine because they’re part of a “normal” diet, but individual tolerance varies widely. The solution isn’t to eliminate entire food groups permanently but to test them systematically.
A structured approach works best. Start by choosing one potential trigger—say, dairy. For one week, consume it regularly and record any symptoms. Then, eliminate it completely for another week, continuing to log how you feel. After the elimination phase, reintroduce it and observe any changes. This method, known as an elimination and reintroduction diet, helps identify true sensitivities without unnecessary restrictions. It’s not about fear or avoidance—it’s about informed choice.
Real-life examples show how powerful this can be. One woman noticed that her morning coffee, paired with milk, consistently led to bloating by midday. After eliminating dairy for a week, the bloating disappeared. Reintroducing it confirmed the link. Switching to a non-dairy alternative brought immediate relief. Another found that gluten-containing bread caused fatigue and brain fog, while gluten-free options did not. These aren’t diagnoses—they’re personal discoveries made through observation.
It’s important to distinguish between food intolerance and food allergy. Intolerances, like lactose intolerance, involve the digestive system and cause discomfort but are not life-threatening. Allergies, such as to nuts or shellfish, involve the immune system and can be dangerous. If you suspect an allergy, consult a doctor before making changes. For intolerances, self-testing is safe and effective. The goal is not perfection but personalization—finding what works for your unique body.
When to Trust Your Gut (And When to See a Pro)
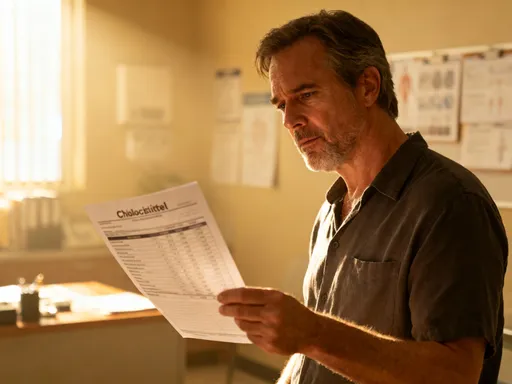
Self-awareness is powerful, but it has limits. There are certain symptoms that should never be ignored, even if they seem minor at first. Unexplained weight loss, chronic abdominal pain, blood in the stool, difficulty swallowing, or persistent vomiting are red flags that require immediate medical evaluation. These could indicate conditions like inflammatory bowel disease (IBD), ulcers, or gastrointestinal cancers, all of which need professional diagnosis and treatment.
Similarly, if self-testing and lifestyle changes don’t improve symptoms after several weeks, it’s time to consult a healthcare provider. A gastroenterologist can order tests—such as blood work, stool analysis, or endoscopy—to identify underlying issues. The data you’ve collected in your symptom journal becomes invaluable here. Instead of saying, “My stomach feels off,” you can say, “I’ve noticed bloating after dairy for three weeks, and my bowel movements are type 6 on the Bristol scale.” This level of detail helps doctors make faster, more accurate assessments.
It’s also important to remember that self-assessment complements, not replaces, medical care. No app, book, or blog can diagnose a condition. But being informed empowers you to ask better questions and participate actively in your health decisions. You are not just a patient—you are a partner in your care. Trusting your gut means honoring both your intuition and the expertise of trained professionals.
Building Daily Habits That Support Stomach Balance
Sustainable gut health comes from small, consistent habits—not drastic overhauls. The most effective changes are simple, science-backed, and easy to maintain. Mindful eating is one of the most impactful. This means sitting down to eat, chewing thoroughly, and avoiding distractions like phones or TV. When you eat mindfully, you activate the parasympathetic nervous system—the “rest and digest” state—which enhances digestion.
Chewing is more important than many realize. Digestion begins in the mouth, where enzymes in saliva start breaking down carbohydrates. Chewing food 20–30 times per bite reduces the workload on the stomach and improves nutrient absorption. It also slows down eating, giving the brain time to register fullness, which helps prevent overeating.
Hydration timing matters too. Drinking water throughout the day supports digestion, but large amounts right before or during meals can dilute stomach acid, making it harder to break down food. The best practice is to drink water 30 minutes before meals and wait at least an hour after eating to avoid interference. Warm water in the morning can gently stimulate digestion and promote bowel movements.
Light movement after meals, such as a 10-minute walk, also aids digestion. Physical activity increases blood flow to the digestive organs and helps move food through the intestines. This is especially helpful for reducing bloating and preventing constipation. These habits don’t require extra time or effort—they fit naturally into daily routines and, over time, create lasting improvements in gut function.
Long-Term Gains: How Small Shifts Add Up
The benefits of paying attention to your gut extend far beyond digestion. When the digestive system works well, energy levels rise, skin becomes clearer, and mood often improves. This is because the gut plays a central role in overall health—it influences immunity, hormone balance, and even brain function. About 70% of the immune system resides in the gut, and the gut-brain axis allows constant communication between the digestive tract and the central nervous system.
Women who adopt gut-friendly habits often report feeling more in control of their health. They sleep better, manage stress more effectively, and experience fewer digestive disruptions. These changes don’t happen overnight, but they are sustainable because they’re built on awareness, not restriction. There’s no need for extreme diets or expensive supplements—just consistent, thoughtful choices.
Listening to your stomach is ultimately an act of self-respect. It’s about honoring your body’s signals and responding with care. In a world that often demands constant giving—whether to family, work, or social obligations—this kind of attention is a quiet rebellion. It says, “I matter. My comfort matters. My health matters.”
Gut health is not a trend or a fad. It’s a lifelong conversation between you and your body. By learning to listen, you gain more than better digestion—you gain a deeper understanding of yourself. And that’s a journey worth taking, one meal, one breath, one mindful moment at a time.