Living Well with Long-Term Health Challenges: My Real Talk on Staying in Control
Living with a chronic condition isn’t about quick fixes—it’s about daily choices that add up. I’ve been there, juggling fatigue, confusion, and fear, wondering if I’d ever feel like *me* again. But over time, small shifts made a real difference. This isn’t a cure—it’s a mindset. With the right habits, support, and self-awareness, managing chronic illness becomes less overwhelming. You’re not alone, and more importantly, you’re still in charge. This journey isn’t about returning to who you were before diagnosis, but about building a new kind of strength—one rooted in resilience, clarity, and intention. The path forward is not always easy, but it is navigable, and it begins with understanding.
Understanding Chronic Conditions: More Than Just a Diagnosis
A chronic condition is not a temporary setback. It’s a long-term health reality—something that persists for months or even years, often for life. Conditions like type 2 diabetes, high blood pressure, arthritis, multiple sclerosis, or thyroid disorders fall into this category. Unlike catching a cold or recovering from a broken bone, where healing has a clear endpoint, chronic illnesses require ongoing attention and care. They don’t simply disappear with a week of rest or a course of antibiotics. Instead, they demand a different kind of relationship with your body—one based on awareness, patience, and consistency.
What makes chronic conditions particularly challenging is their invisible nature. Many symptoms—fatigue, brain fog, joint pain, digestive discomfort—aren’t obvious to others. This can lead to misunderstandings, even from loved ones who care. A woman with fibromyalgia might look perfectly healthy but struggle to get out of bed some days. Someone managing Crohn’s disease may need to cancel plans at the last minute due to a flare-up. These experiences can breed isolation, as the person feels misunderstood or dismissed. Over time, the emotional burden can become as heavy as the physical symptoms.
Equally important is recognizing that a diagnosis is not a life sentence of decline. While chronic conditions are long-lasting, their impact is not fixed. How they affect daily life depends largely on how they are managed. For example, someone with hypertension who adopts a heart-healthy diet, exercises regularly, and takes medication as prescribed often maintains excellent cardiovascular health for decades. The condition is present, but its consequences are minimized. This shift—from seeing illness as an identity to viewing it as a manageable part of life—is foundational to long-term well-being.
It’s also crucial to acknowledge the mental toll. Living with uncertainty—wondering when the next flare-up will come, how it will affect your day, or whether your energy will hold—can fuel anxiety. Feelings of frustration, grief, or even guilt are common. You might think, “Why can’t I just push through?” or “I should be stronger.” But these thoughts often come from a place of misunderstanding. Chronic illness is not a failure of willpower. It’s a complex interplay of biology, environment, and lifestyle. Accepting this truth is not defeat—it’s the first step toward empowerment.
The Mindset Shift: From Survival to Strategy
When first diagnosed, many people fall into a reactive pattern—waiting for symptoms to worsen before taking action. This survival mode feels natural. If pain flares, you rest. If blood sugar spikes, you adjust your meal. But this cycle keeps you one step behind, constantly responding rather than leading. The shift to proactive management changes everything. It means treating your health not as a series of emergencies, but as a daily practice—like brushing your teeth or locking the door at night. Small, consistent actions prevent bigger problems down the line.
One powerful way to make this shift is by reframing how you see your daily routines. Taking medication every morning might feel like a reminder of illness, but it can also be seen as an act of self-respect—an investment in your future. Checking your blood pressure or glucose levels isn’t about fear; it’s about information. Movement isn’t punishment for being unwell—it’s a gift to your body, helping it stay strong and resilient. These mental reframeings don’t erase the difficulty, but they restore a sense of agency. You’re not just enduring your condition—you’re actively shaping how it affects you.
Acceptance is often misunderstood as giving up. In reality, it’s the opposite. Acceptance means acknowledging the facts of your situation without fighting them. It’s saying, “Yes, I have this condition, and it affects me, but I still have choices.” From this grounded place, you can make decisions based on reality, not denial or despair. Denial leads to avoidance—skipping doctor visits, ignoring symptoms. Despair leads to inaction. But acceptance creates space for action. It allows you to ask, “Given my condition, what can I do today to feel better?” That question is the starting point of control.
This mindset also helps reduce shame. Many people feel embarrassed by their limitations—needing to sit down during a family gathering, turning down invitations, or asking for help. But reframing these actions as necessary and wise, rather than weak, changes their emotional weight. Choosing to rest when tired isn’t laziness—it’s wisdom. Saying no to overcommitment isn’t selfish—it’s self-protection. These choices reflect strength, not failure. Over time, this internal dialogue becomes kinder, more supportive, and far more empowering.
Building Your Daily Health Routine: Small Steps, Big Impact
When managing a chronic condition, consistency matters more than intensity. You don’t need to run marathons or overhaul your entire diet overnight. What helps most is building sustainable habits—small, repeatable actions that become part of your daily rhythm. Think of these habits as building blocks. One block alone may not seem like much, but over time, they create a solid foundation for better health.
Nutrition is a key pillar. Eating balanced meals with whole grains, lean proteins, healthy fats, and plenty of vegetables helps stabilize energy and supports immune function. For someone with diabetes, consistent carbohydrate intake helps manage blood sugar. For those with inflammatory conditions, reducing processed foods and added sugars may help lower flare-ups. Meal prepping—even just chopping vegetables or cooking a batch of quinoa on weekends—can make healthy choices easier during busy days. It’s not about perfection. A nourishing breakfast one day and a simpler option the next is still progress.
Movement is another essential piece. Physical activity doesn’t have to mean gym sessions or intense workouts. Gentle movement—walking, stretching, yoga, or water exercises—can improve circulation, reduce stiffness, and boost mood. For someone with joint pain, short walks around the block may be more sustainable than long hikes. The goal is regularity, not performance. Even ten minutes a day can make a difference over time. The key is finding activities that feel good and can be maintained, not pushed through in pain.
Sleep and stress management are equally important. Poor sleep can worsen inflammation, increase pain sensitivity, and disrupt hormone balance. Creating a calming bedtime routine—dimming lights, avoiding screens, reading, or practicing gentle breathing—can improve sleep quality. Stress, too, plays a major role in chronic conditions. High cortisol levels can trigger flares in autoimmune disorders or raise blood pressure. Simple techniques like deep breathing, mindfulness, or journaling can help regulate the nervous system. These practices don’t eliminate stress, but they build resilience against its effects.
The beauty of these habits is that they compound. One day of walking may not change much, but thirty days of walking can improve endurance, mood, and confidence. One healthy meal won’t reverse a diagnosis, but a pattern of nourishing choices supports long-term stability. The focus should never be on dramatic results, but on showing up for yourself, day after day. Progress, not perfection, is the true measure of success.
The Power of Monitoring: Tracking to Take Control
Self-monitoring is one of the most powerful tools in managing chronic conditions. When you track your symptoms, energy levels, food intake, or medication effects, you gain valuable insights. Patterns begin to emerge—perhaps you notice fatigue after eating certain foods, or joint pain increases during periods of high stress. These observations help you understand your body’s signals and respond more effectively. Instead of guessing, you’re making informed decisions.
Tracking doesn’t have to be complicated. A simple notebook, a printed chart, or a digital app can work. The goal is consistency, not complexity. Some people find it helpful to rate their energy or pain on a scale of 1 to 10 each day. Others log meals, sleep duration, or medication times. Over weeks or months, these records can reveal trends that might otherwise go unnoticed. For example, a woman with migraines might discover that skipping breakfast often precedes a headache. With this knowledge, she can take preventive steps.
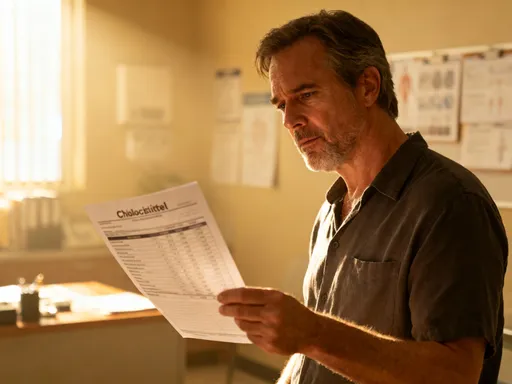
This data also strengthens communication with healthcare providers. Instead of saying, “I’ve been feeling off,” you can say, “My fatigue has been a 7 or 8 most days this week, and I’ve noticed it’s worse after eating gluten.” Specific, documented information helps doctors make better recommendations. It transforms vague complaints into actionable insights. Providers appreciate patients who come prepared with observations, as it supports more accurate assessments and personalized care.
Monitoring also fosters a sense of control. When you feel overwhelmed by symptoms, looking back at your records can provide perspective. You might realize that bad days are less frequent than they feel, or that a new medication is starting to help. This evidence-based awareness reduces fear and builds confidence. It reminds you that you’re not powerless—that you’re gathering knowledge to guide your choices. Over time, tracking becomes less about counting symptoms and more about understanding your unique health rhythm.
Teamwork Matters: Working with Healthcare Providers
Managing a chronic condition is not a solo journey. While self-care is essential, it works best when combined with professional guidance. Your healthcare team—doctors, nurses, specialists, dietitians, physical therapists, or mental health counselors—plays a vital role in your care. They bring expertise, experience, and access to treatments you can’t manage on your own. The key is building a collaborative relationship, one based on mutual respect and open communication.
Effective collaboration starts with preparation. Before appointments, take time to review your symptom logs, list your concerns, and write down questions. This ensures you don’t forget important topics in the moment. For example, instead of vaguely asking, “Is this normal?” you might say, “I’ve had tingling in my hands for three weeks—could it be related to my medication?” Specific questions lead to specific answers. Bringing your tracking records to appointments also helps providers see the full picture.
Don’t hesitate to ask for clarification. Medical terms can be confusing, and treatment plans aren’t always clear. If a doctor recommends a new medication, ask about its purpose, dosage, potential side effects, and how long it might take to work. If a dietitian suggests dietary changes, ask for practical examples or resources. You have the right to understand your care. If something feels unclear or overwhelming, say so. A good provider will welcome your questions and adjust their explanations to meet your needs.
It’s also okay to seek a second opinion or switch providers if the relationship isn’t working. You deserve care that feels supportive, not dismissive. Trust your instincts. If a doctor minimizes your symptoms or rushes through appointments, it’s valid to look for someone who listens. Building a care team you trust takes time, but it’s worth the effort. When you and your providers work together, care becomes more personalized, effective, and aligned with your goals.
Emotional Wellness: Protecting Your Mental Energy
Chronic illness doesn’t just affect the body—it affects the mind. The constant effort of managing symptoms, appointments, and lifestyle changes can lead to emotional burnout. Feelings of sadness, irritability, or numbness are not signs of weakness; they’re common responses to ongoing stress. Many women in their 30s, 40s, and 50s report feeling “tired of being tired,” or grieving the loss of their former energy and independence. These emotions are real and deserve attention.
One of the most important things you can do is protect your mental energy. This means setting boundaries, pacing yourself, and making space for rest. It might mean declining extra responsibilities at work or home, or asking for help with chores. It might mean scheduling quiet time during the day, even if it’s just ten minutes with a cup of tea and no distractions. These choices aren’t indulgent—they’re necessary for emotional sustainability.
Mindfulness and journaling can also support emotional health. Mindfulness involves paying attention to the present moment without judgment. It doesn’t erase pain, but it can reduce the struggle against it. Simple practices—focusing on your breath, noticing sounds around you, or observing your thoughts—can create moments of calm. Journaling offers a safe space to express fears, frustrations, and hopes. Writing down your thoughts can help you process them, gain clarity, and release emotional tension.
Staying socially connected is another vital piece. Isolation worsens emotional strain. Even small interactions—calling a friend, joining a support group, or chatting with a neighbor—can boost mood and reduce feelings of loneliness. Support groups, whether in person or online, offer a unique kind of understanding. Talking with others who “get it” can be incredibly validating. You’re not alone in your experience, and hearing how others cope can inspire new strategies.
If emotional strain becomes overwhelming, seeking professional help is a sign of strength, not failure. Therapists, counselors, or psychologists can provide tools to manage anxiety, depression, or adjustment difficulties. Cognitive behavioral therapy (CBT), for example, helps identify unhelpful thought patterns and replace them with more balanced ones. Mental health care is not a luxury—it’s an essential part of overall health, especially when living with long-term conditions.
Looking Ahead: Creating a Sustainable Life, Not Just a Survival Plan
Living well with a chronic condition isn’t about returning to how things used to be. It’s about creating a new kind of normal—one that honors your limits while still allowing for joy, connection, and purpose. The goal is not just to survive, but to thrive in the life you have now. This means setting goals that matter to you, whether that’s traveling with family, gardening, volunteering, or simply enjoying quiet mornings with a book. These moments of fulfillment are not distractions from health—they are part of it.
Adaptation is key. You may need to adjust how you do things, but that doesn’t mean giving up on them. Want to go on a family trip? Plan rest stops, pack medications, and choose accommodations with accessibility in mind. Want to host a holiday dinner? Prepare dishes ahead, ask for help, and focus on what brings you joy. These adjustments aren’t limitations—they’re strategies for inclusion. They allow you to participate fully, on your own terms.
Over time, this approach builds resilience. You learn what your body needs, how to pace yourself, and when to ask for support. You develop a deeper understanding of your strengths and limits. And you discover that a fulfilling life isn’t defined by the absence of illness, but by the presence of meaning, connection, and self-compassion. Chronic doesn’t have to mean confined. With awareness, support, and steady effort, you can live a balanced, satisfying life—one day at a time.
Always remember: this guide is not a substitute for professional medical advice. Every individual’s health journey is unique. Consult qualified healthcare providers to develop a plan tailored to your needs. But know this—you are not powerless. You have more control than you think. By making informed choices, building supportive habits, and honoring your experience, you remain the author of your life. And that, more than anything, is worth celebrating.